Public Health professionals have been in the spotlight for their work around the COVID-19 pandemic. You’ve heard all about the testing sites, call centers, and vaccination clinics. They’re also the ones on the other end of the phone (or screen) answering your questions about the virus – how can I protect myself? What should I do if I think I have COVID-19? Is the COVID-19 vaccine safe? (Yes, it’s safe and effective! Learn more here.) They are real life HEROS, and our community owes them all a huge THANK YOU!
The reality is, Public Health professionals track epidemics every day, and while the job isn’t always as glamorous as Hollywood would suggest (have you seen Contagion!?), it is an essential public health service. It’s one of 10 essential services, in fact.
10 Essential Services of Public Health
Here’s a peek at what public health professionals do every day for our community (pandemic or not):
1. Monitor Community Health
Data is critical for all public health services. Without it, we wouldn’t know what’s need in our community, where priorities should lie, or how to allocate resources effectively. There are systems all over the world (and locally) to help sound alarms if something goes wrong. Monitoring the health status of a community includes looking at things like injuries, chronic diseases, and birth outcomes to see what trends — if any — exist. This service so important. After all, before public health officials can do anything to improve the health of a community, they must first figure out what the community’s needs are.
2. Investigate Health Problems and Hazards in the Community
Once a health problem has been identified, public health officials work to figure out who is most impacted and why. Epidemiologists collect and analyze data to figure out how diseases or health conditions are distributed in a given population, and what key factors those cases have in common. And — most importantly — how that information could be applied to prevent future cases. Real life example: When there’s a salmonella outbreak, epidemiologists are the ones talking to those who got sick, collecting information on what they ate, and pinpointing what food is the likely culprit so that it can be pulled from the shelves.
3. Inform, Educate, and Empower People About Health Issues
Once public health professionals know what’s going on, who it’s impacting, and — if possible — how to prevent it, they then spread the word to the population at large. Real life example: The Back to Sleep campaign. Epidemiologists around the world started to identify sleep position as a risk factor for Sudden Infant Death Syndrome (SIDS). So, health officials launched a national educational campaign urging parents to place babies on their backs to sleep, rather than on their stomachs or sides. Pediatricians talked about it with their patients’ families, pamphlets were passed out, and experts went on television to spread the word. And it looks like it worked. SIDS rates dropped by over 50 percent in the years immediately following the launch of the campaign.
4. Partner With the Community to Work on Health Problems

Public Health relies on the cooperation and support of a wide variety of stakeholders to investigate, resolve, and prevent health issues. That could even include people and organizations who may not be involved in health directly. Partners of all kinds can be crucial to gathering accurate information and empowering people to adopt certain behavior changes. Real life example: Public health has gotten help from local people and groups to help combat HIV in marginalized populations. Instead of using authority figures to disseminate key information, programs work within peer networks to reach those most at risk for infection. After all, who better to help influence positive change in a community than the people who are already a part of it?
5. Develop Policies and Plans that Support Individual and Community Health
Some of the greatest public health achievements were not due to one-on-one education or small, local efforts. They were a result of policy changes. Real life examples: Workplace safety guidelines, seat belt laws, and minimum quality standards for drinking water, all led to significant improvements to our health and safety.
6. Enforce Laws that Protect Health and Ensure Safety
Health codes help prevent food-borne illness by requiring restaurants to keep certain standards. But, would they be as effective if health officials never came out to inspect the kitchens? Probably not! Policies can lead to health improvements for many people in a community, but only if they are enforced.
7. Connect People to the Personal Health Services They Need
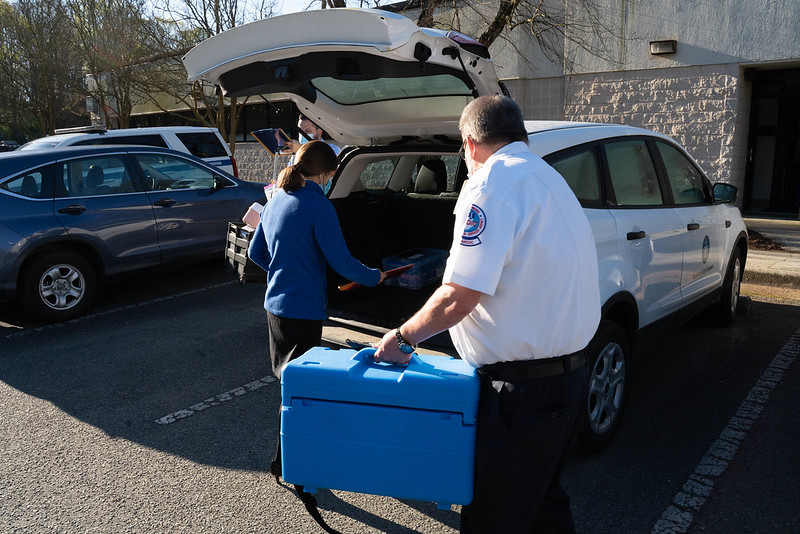
Access to health care can be complicated. Whether you’re able to see a doctor when needed could depend on a lot of factors, including your age, location, financial situation, health condition, and employment status. Public health agencies help make sure some of the most vulnerable populations in a community can access health care. And access doesn’t just mean getting in to see a doctor. It can also mean having transportation to and from medical services, affordability of the care provided, and culturally-appropriate translations. Real life example: The health department runs WIC (the Special Supplemental Nutrition Program for Women, Infants, and Children). The program helps ensure that all kids, regardless of income, have access to good nutrition in the first few years of life.
8. Assure Competent Public and Personal Healthcare Workforce
Medicine is always changing to adapt to the latest research and available technologies. Medical professionals are required to take classes to stay up to date. Local health departments collaborate with medical associations to offer continuing education classes on a wide range of topics. This could include courses on bioterrorism and emergency preparedness. Yes, responding to natural disasters falls under public health, too.
9. Evaluate Effectiveness of Health Programs
Public Health has to monitor initiatives constantly to verify they actually work. Programs that require funding are also assessed to make sure resources are being used appropriately. To do this, health economists help estimate the cost-effectiveness of a given policy change. Epidemiologists look at disease trends among participants of a particular health initiative to see if they’ve improved. Biostatisticians look at data from surveys and medical records to determine whether certain health indicators in a given population have changed. The results from these evaluations help to improve programs.
10. Research Innovative Solutions
One of the most important ways public health works to protect the health and safety of a community is through asking questions, gathering data, and finding new and better ways to solve problems. Real life examples: Public health research on vehicular crashes brought us safer cars and seat belts. Investigations of a dental anomaly led to fluoride in drinking water. Understanding our immune system resulted in developing vaccines that have saved millions of lives and billions of dollars.
So not only do public health professionals lead the way and work to keep us safe during times of crisis (like we’ve recently experienced), but they’re also always working to better us as individuals and as a community. The work isn’t glamorous, but it’s pretty amazing.